Blood smear evaluation is an often overlooked, but very important, aspect of an in-house haematology.
With the advancement in haematology analysers that can now detect reticulocytes and even band neutrophils, some practitioners are beginning to rely solely on the numerical data alone in evaluating the patient’s blood.
The art of blood smear interpretation is on the decline. However, it is an extremely valuable skill that must be practised and perfected and really should be part of every in-house haematology.
Plus points
What are the benefits of being good at blood smears?
- Identifying a regenerative response, looking for reticulocytes (polychromatophils).
- Looking for other possible causes of an anaemia – such as Heinz bodies, infectious microorganisms or spherocytes, which can indicate an immune-mediated haemolytic anaemia.
- Confirming thrombocytopenias, as frequently platelet clumping can be reported as a thrombocytopenia.
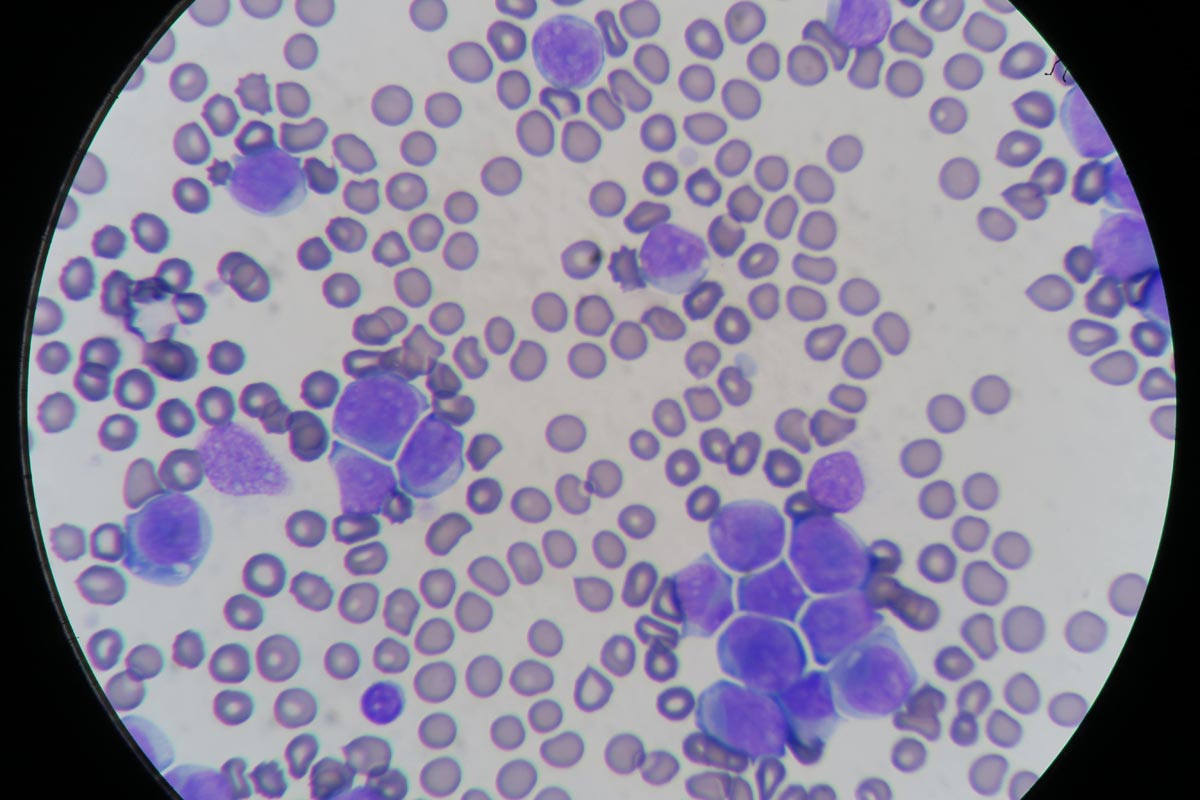
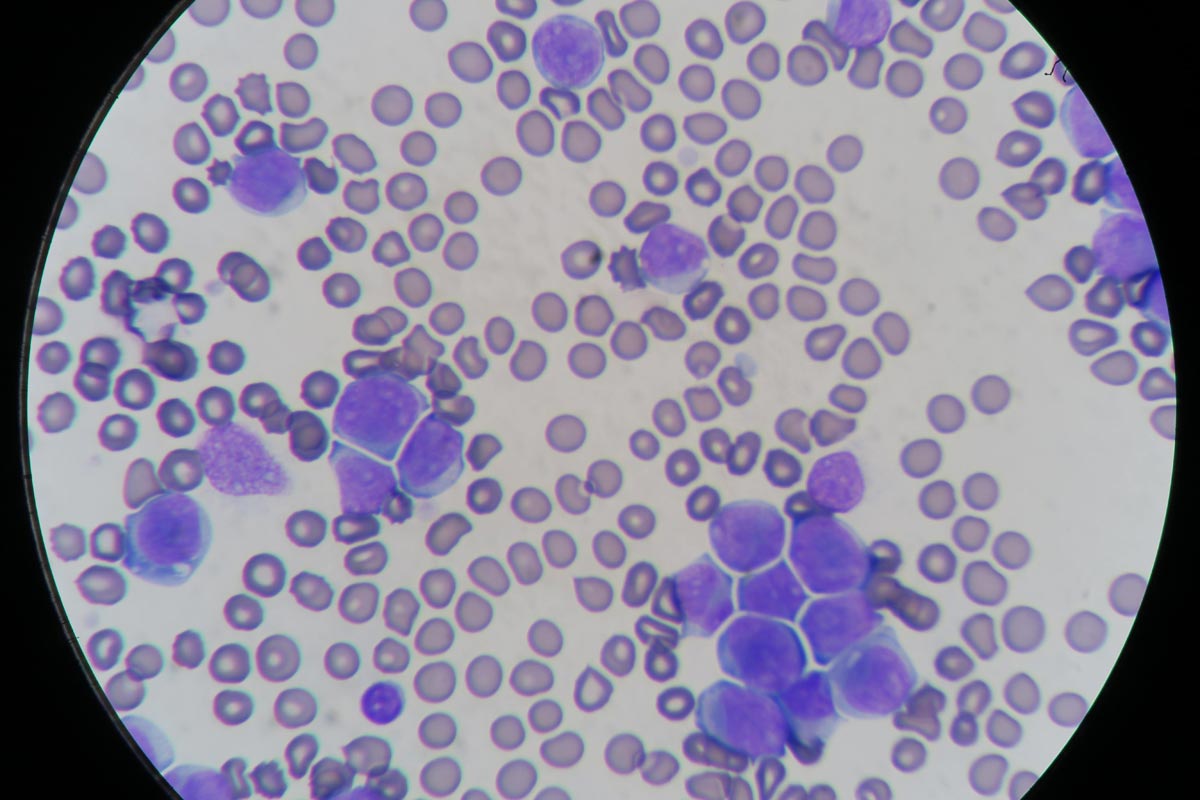
- Assessment of the nature of a leukocytosis. High leukocyte counts do not always mean infection. Neutrophilia can be caused by both elevated immature and mature neutrophils. Determining the nature of neutrophilia can provide crucial information in identifying the underlying cause and if the patient is coping or not. Apart from infection, other causes can include stress, corticosteroids and neoplastic leukaemias.
- Normal leukocyte counts do not always mean the patient is okay. Patients can have severe left shifts, but normal leukocyte counts.
Practice makes perfect
Blood smear evaluation begins with becoming accomplished at producing great diagnostic smears. This takes practice; poorly performed smears can be non-diagnostic and frustrating to assess for both yourself and an external pathologist.
A few tips on the technique:
- Use a very small drop of blood. If you have picked up too much blood with the “spreader” slide, lift off and start the smear away from that drop of blood.
- Angle the “spreader” slide about 30°. The bigger the angle, the shorter your smear.
- Push the “spreader” slide forward.
- The smear should end at about half to three-quarters of the way down the slide and must have a “feathered edge”.
Leave a Reply