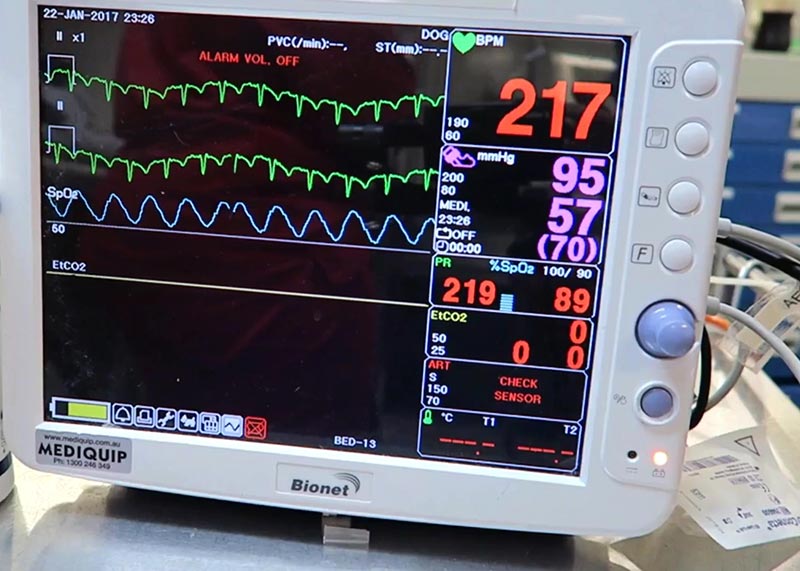
With the widespread availability of pulse oximetry and its relative ease of use, it’s easy to become complacent and overly reliant on its values.
One must remember pulse oximetry is only an indirect measurement of the arterial haemoglobin saturation, so these values are based on a series of assumptions on the other important factors that determine oxygenation.
To understand the overall oxygen status of a patient, you will need to assess the pulse oximetry values in the context of the oxyhaemoglobin dissociation curve (OHDC).
SaO2 and PaO2
The OHDC depicts the relationship between oxygen saturation of haemoglobin (SaO2) and the partial pressure of arterial oxygen (PaO2). However, before discussing the interpretation of the OHDC graph, we must understand the difference between SaO2 and PaO2:
- SaO2 refers to the percentage of haemoglobin molecule within red blood cells that is bound to oxygen. Each haemoglobin molecule is made up of four strands of amino acids, each of which are able to bind to one molecule of oxygen. When these binding sites are fully saturated (bound), this is reflected as 100% oxygen saturation.
- PaO2 is the partial pressure of oxygen dissolved in blood (expressed in mmHg) – or, more simply put, the measurement of oxygen content in arterial blood. The higher the PaO2, the more readily oxygen binds to haemoglobin.
Influences
Aside from SaO2 and PaO2, other important elements exist that determine the effectiveness of oxygenation of tissue, both in terms of oxygen delivery and oxygen dissociation (offloading from haemoglobin).
The efficiency of oxygen transport is influenced by:
- the number of haemoglobin molecules available for oxygen uptake
- a sufficient blood volume
- a competent circulatory system (cardiac output and blood pressure)
Oxygen dissociation from haemoglobin molecules to the target tissue is directly determined by the tissue demand for oxygen.
It should be noted none of these factors are assessed by the pulse oximeter, thus highlighting the limited value of pulse oximetry in the absence of the knowledge of these other factors and the context of the OHDC.
So, the first key point is the number displayed on the pulse oximeter should not be interpreted in isolation.
The goal of the next couple of posts is to help you understand the limitations of pulse oximeters, what the OHDC means, what factors can affect this curve, and how to interpret pulse oximetry values in the context of the curve to get a more accurate picture of the patient’s overall oxygenation status.

Leave a Reply