In various disease and physiological states, the oxyhaemoglobin dissociation curve (OHDC) can shift either left or right. This indicates the increase, or decrease, of the haemoglobin’s (Hgb’s) affinity to oxygen, respectively.
It is important to recognise the situations in which this happens, to manage patients effectively.
Right shift
A shift of the OHDC to the right indicates the Hgb has a reduced affinity to oxygen. This is normally seen in environments where oxygen needs to be released by the Hgb molecules – for example, muscles and placenta.
Four major factors influence this:
- low blood pH (lactic acid)
- high temperature – especially working muscles
- high partial pressure of carbon dioxide (PCO2)
- increased 2,3-bisphosphoglycerate (2,3-DPG) – an intermediate of glycolysis
2,3-DPG
2,3-DPG is produced in red blood cells during glycolysis. Its production is increased for several conditions in the presence of diminished peripheral tissue oxygen availability, such as hypoxaemia, chronic lung disease, anaemia and congestive heart failure. It promotes oxygen to be released into the tissues and, therefore, makes it harder for oxygen to bind with Hgb in the lungs.
The presence of 2,3-DPG can increase oxygen release to the tissue equivalent to that if the surrounding arterial partial pressure of oxygen (PaO2) was 10mmHg higher. This is why 2,3-DPG is increased during pregnancy to increase oxygen delivery to the growing fetus.
Another example is during exercise – in the presence of high CO2 and more hydrogen ions (H+) from lactic acid (lowering the pH), the curve is shifted to the right to help increase oxygen release in the muscles.
Left shift
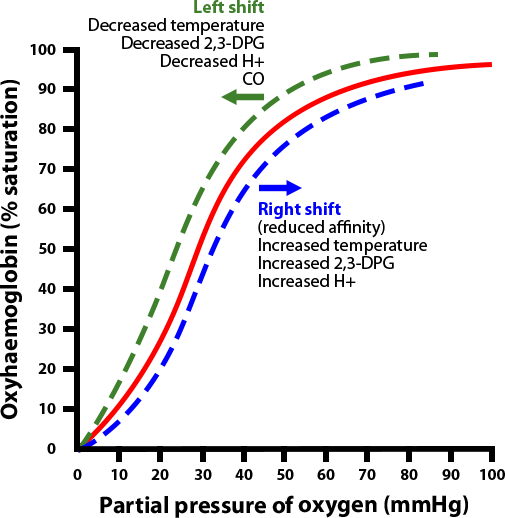 By the same token, a shift of the curve to the left means the Hgb has an increased affinity for oxygen, so is less likely to release it to the tissue. This normally occurs in the lungs.
By the same token, a shift of the curve to the left means the Hgb has an increased affinity for oxygen, so is less likely to release it to the tissue. This normally occurs in the lungs.
The factors this promotes are:
- high blood pH (breathing off CO2 – an acid)
- low temperature (ambient temperature usually lower than that of the lungs)
- reduced PCO2 (ventilation)
- decreased 2,3-DPG and the presence of fetal Hgb
So, during exercise, in the presence of lower CO2 and less H+, the curve shifts to the left to help increase oxygen uptake into the Hgb.
Carbon monoxide toxicity
One pathological situation that causes a left shift of the curve is carbon monoxide (CO) toxicity.
Not only does it cause the OHDC curve to shift to the left, but the Hgb is also 240 times more likely to bind to CO than oxygen. The situation is further complicated by pulse oximeters’ inability to differentiate CO-bound Hgb to O2-bound Hgb, therefore giving a false reading of normal partial pressure of oxygen in the face of severe hypoxaemia. Similarly, methemoglobinaemia has a similar effect to CO and causes a left shift of the OHDC.
Conclusion
Understanding the relationships between Hgb, oxygen saturation, PaO2 and the causes of the shifts of the curves will allow accurate assessments of patients.
For example, a patient with unusual hypoxaemia derived from arterial blood gas – despite normal PaO2 and peripheral oxygen saturation – will immediately increase the suspicion of CO toxicity.
Similarly, a patient presenting with shortness of breath, despite adequate ventilation and oxygen saturation, will suggest Hgb deficiency.
Leave a Reply