Monitoring devices are crucial in the success of cardiopulmonary resuscitation (CPR).
Many monitoring modalities can be used during CPR for the assessment of the adequacy of CPR efforts and the return of spontaneous circulation (ROSC). These monitoring devices, however, should never be used as a sole mechanism to confirm cardiopulmonary arrest. Indeed, commencement of CPR should not require any further prompting than the suspicion of cardiopulmonary arrest (CPA).
Of the numerous monitoring modalities examined, only ECG and end tidal carbon dioxide (ETCO2) monitoring are associated with positive CPR outcomes.
CPA precautions
As mentioned in the first part of this series of CPR blogs, we often have this crippling urge to confirm CPA before starting CPR – this must be stopped.
While femoral pulse palpation, electrocardiography, absence of pulse identified by a Doppler ultrasonic flow probe, and ETCO2 monitoring can all help diagnose non-perfusing cardiac rhythms or CPA, we should not turn to these to verify a CPA event – obviously with the exception of anaesthetised animals that are already connected to these devices.
Accurate and swift determination of the presence of a pulse is often unreliable, even for trained health care professionals. This process often takes more than 10 seconds – and longer if Doppler, or other monitoring equipment, are used. Additionally, in the absence of other supportive evidence of CPA – such as apnoea, agonal breathing or lack of an auscultable heartbeat – the absence of a pulse cannot be used to definitively diagnose CPA.
ECG rhythms, while effective in diagnosing asystole, fibrillation patterns and arrhythmia, can be misleading – especially in the case of pulseless electrical activity (PEA).
ETCO2 can only be monitored once a patient is intubated, rendering it useless in the non-anaesthetised and intubated patient. Once a patient is intubated, it should never be used to determine correct placement of ET tubes, as ETCO2 will approach zero when cessation of cardiac output occurs.
Since the aforementioned monitoring methods take a substantial amount of time and are thus detrimental to the success of achieving ROSC, you should not need any further clinical signs beyond apnoea and unresponsiveness in a patient to start CPR.
ECG monitoring
 ECG monitoring is beneficial for identifying the initial arrest rhythm pattern, as well as being used as an ongoing monitoring device.
ECG monitoring is beneficial for identifying the initial arrest rhythm pattern, as well as being used as an ongoing monitoring device.
Veterinary patients in CPA often are in asystole or have PEA, both of which will convert to ventricular fibrillation (VF) in the majority of cases. As VF and ventricular tachycardia (VT) are both amenable to defibrillation (shockable rhythms), it is critical to use ECG as an ongoing monitoring device to identify these patterns and detection of conversions after defibrillation.
That being said, monitoring of ECG should never interrupt chest compression cycles, as the risk of affecting cardiac perfusion pressure outweighs this benefit. In fact, in a retrospective study, 73% of patients redeveloped VF by 60 seconds after defibrillation (Blouin et al, 2001), indicating rhythm analysis immediately after defibrillation is not accurate in determining defibrillation success.
In addition to this, minimisation of hands-off time after defibrillation for rhythm check appears to improve CPR outcome; therefore, it is prudent to resume chest compression as soon as possible after defibrillation and rhythm identification.
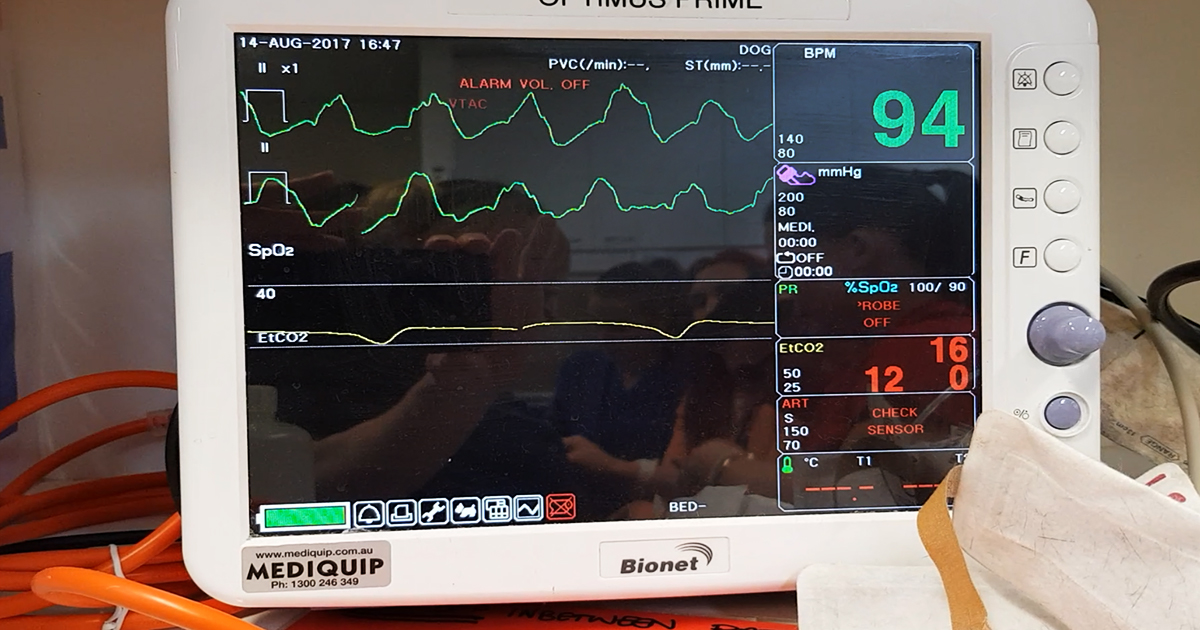
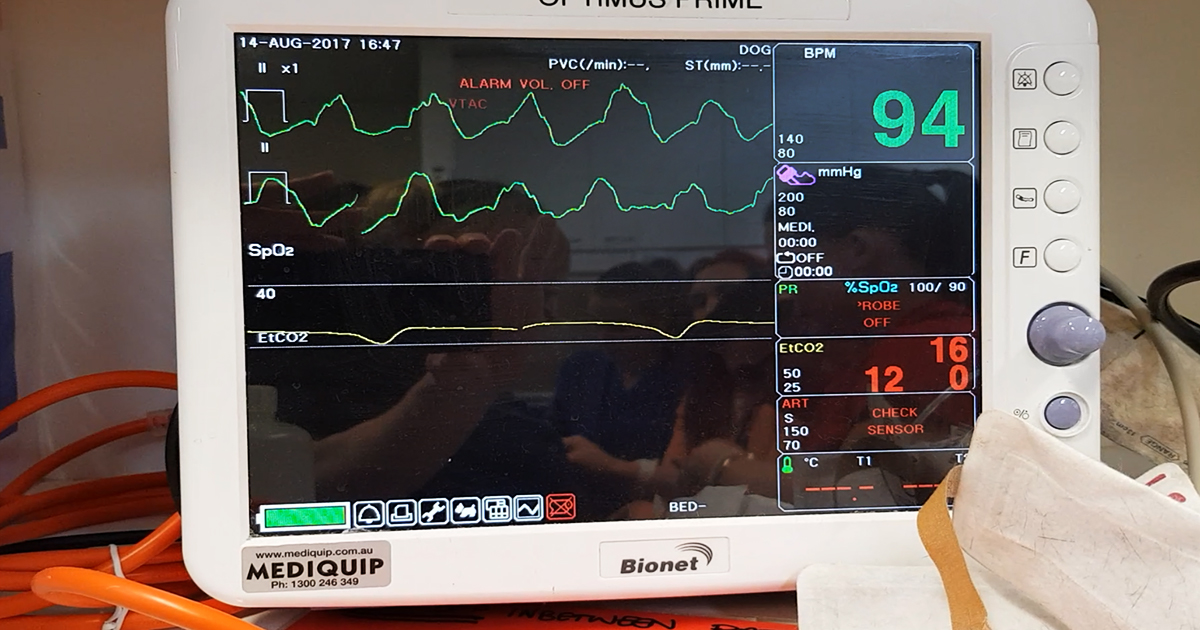
ETCO2 measurement
ETCO2 measurement is an invaluable tool in monitoring during CPR and is integral to the success of CPR.
ETCO2 measurements during CPR indirectly measures cardiac output, cardiac index, coronary perfusion pressure and mean aortic pressure, and thus is a surrogate indicator of the quality of CPR. Higher ETCO2 readings over the course of CPR are reflective of high-quality compressions and more likely to achieve ROSC, survive to hospital discharge, or both.
Despite this, the optimal ETCO2 values in veterinary patients (to achieve ROSC) have not been determined as yet. As a general rule, ETCO2 greater than 15mmHg is indicative of effective CPR. Therefore, the ETCO2 measurement can only be used as a guide to optimise CPR techniques to improve the likelihood of ROSC.
While monitoring equipment can be used to confirm CPA and assist further treatment planning, these should never be used in lieu of immediate chest compressions. ECG is crucial in diagnosing shockable rhythms and general cardiac rhythm monitoring, while ETCO2 gives information on the quality of the chest compressions.
Substantial evidence exists that the use of these two monitoring modalities improves the chances for ROSC (Gudipati et al, 1988; Trevino et al, 1985) and, therefore, should be incorporated into the standard CPR protocol.
Leave a Reply