As discussed in part 1 and part 2 of this series, many dogs and cats can recover from severe brain injuries if systemic and neurological abnormalities are identified and managed appropriately and early enough.
The initial trauma to the brain parenchyma is followed by secondary damage resulting from haemorrhage, ischaemia and oedema. As the brain is enclosed within the bones of the skull, the intracranial pressure (ICP) increases due to brain tissue oedema or haemorrhage, leading to decreased cerebral perfusion and further brain damage.
We have covered the several aspects of the management of a patient with brain injury previously, but the focus of this post is around the use of hypertonic saline and mannitol in reducing cerebral oedema.
Hypertonic saline
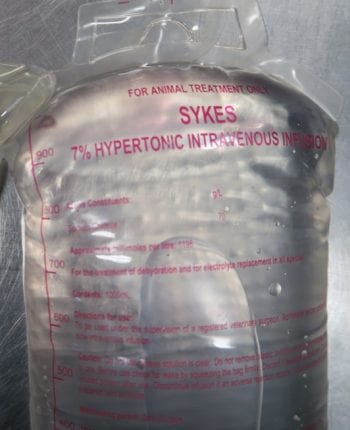
The first and most important point is you can use either hypertonic saline (HTS) 7% or mannitol. Some recent studies have shown HTS is superior to mannitol in decreasing cerebral oedema.
In one study, HTS maintained better cerebral perfusion in the early phase of therapy, but no significant difference in systemic haemodynamics existed between the two.
- 7% NaCl; 4ml/kg in dogs and 2ml/kg in cats slow IV over 10 to 15 minutes
HTS allows rapid restoration of blood volume and blood pressure, while limiting the volume of fluid administered. It does this by drawing fluid from the interstitial and intracellular spaces into the intravascular space, and this results in increased cerebral blood pressure and flow.
This draw of fluid can reduce cerebral oedema and subsequent intracranial pressure; it is also thought to reduce the distance oxygen has to diffuse across improving oxygen delivery to damaged tissues. Other possible beneficial effects include modulating the immune response and reducing the release of excitatory neurotransmitters release from damaged brain tissue.
HTS should be avoided in case the patient is systemically dehydrated or hypernatraemic. The effects of HTS are short term – only one hour. Because it can increase sodium concentrations rapidly, it is recommended to be delivered only once and that another isotonic crystalloid should be administered during or shortly after the administration of HTS to prevent dehydration.
Mannitol
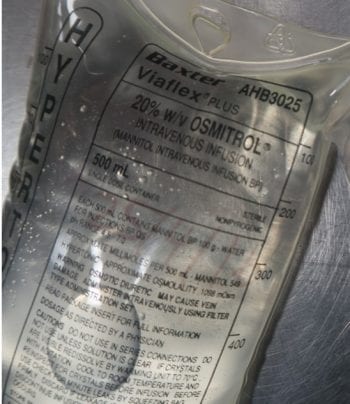
- 0.25mg/kg to 1mg/kg IV over 20 minutes
- Repeat mannitol every 4 hours as needed
Mannitol is an osmotic diuretic; however, its immediate effect is blood volume expansion, resulting in increased cerebral blood flow and oxygen delivery. It also results in reduced blood viscosity, leading to a short-term vasoconstriction of the cerebral blood vessels that, within a few minutes, can cause a reduction in ICP.
The slower onset osmotic effect reverses the blood-brain osmotic gradient, thereby reducing extracellular fluid volume in both normal and damaged brain, leading to reduced ICP.
Mannitol should be administered as a bolus over a 15-minute period, rather than as an infusion, to obtain the blood volume expanding effect. Its brain oedema-reducing effects can take approximately 15 to 30 minutes to establish and last for 2 to 5 hours.
Administering doses of 0.25mg/kg appear equally effective in lowering ICP as doses of 1mg/kg, but may last a shorter period of time.
Repeated administration of mannitol can cause an accompanying diuresis, which may result in blood volume loss, intracellular dehydration and, if not managed, can lead to reduced blood pressure. Mannitol is contraindicated if the patient is dehydrated, or in anuric kidney failure or congestive heart failure.
Some resources recommend it should not be given patients with intracranial haemorrhage, but this is often impossibly to determine in veterinary patients without advanced imagery, and the generally consensus is its benefits out weight the risk of mannitol leakage and possible increased intracranial pressure.
To summarise
My general approach to head trauma is as follows:
- Correct any perfusion or hydration deficits – consider saline 0.9%
- Treat any suspected ICP with mannitol or HTS
- Provide supplemental oxygen
- Administer pain relief – a pure opioid is preferred; for example, methadone or fentanyl constant rate infusion
- 15° to 30° degree cranial body elevation
- Avoid any pressure on the jugular region
- Assess Modified Glasgow Coma Scale on presentation, then 30 minutes, 60 minutes then every 4 hours.
- Constant monitoring of vital parameters, pulse oximetry, partial pressure of carbon dioxide (or end-tidal CO2) and blood pressure
- Consider not actively rewarming the patient if it is mildly hypothermic
- Mechanical ventilation, if hypercapnia is present greater than 50mmHg, and the patient is not improving and all other options have failed.
- Blood transfusion if PCV less than 25

Leave a Reply